
IBS is a very common health problem among the population in the western world. The syndrome is characterized by disruption of bowel function and motility without evidence of structural defects.
The syndrome is more common in women than men. The symptoms vary from person to person and can manifest in a wide range; From mild symptoms that do not affect one's lifestyle at all to severe symptoms that greatly affect the quality of life.
There is no specific test in place to check for irritable bowel syndrome while the diagnosis of the same is feasible by negating other illnesses that can cause the same symptoms (food intolerance, celiac disease, various infections, various bowel diseases, and more).
The causes of irritable bowel syndrome are unclear and are attributed to physiological aspects (such as structural impairment), psychological (such as stress, anxiety, and depression), and dietary ones (processed foods and deficiency in gut-friendly bacteria).
How Microbiome Testing Can Transform Your IBS Experience
Living with Irritable Bowel Syndrome can feel like your gut has a mind of its own. The unpredictable cramping, bloating, and bathroom urgency can rule your life, making simple outings stressful and uncomfortable days all too common.
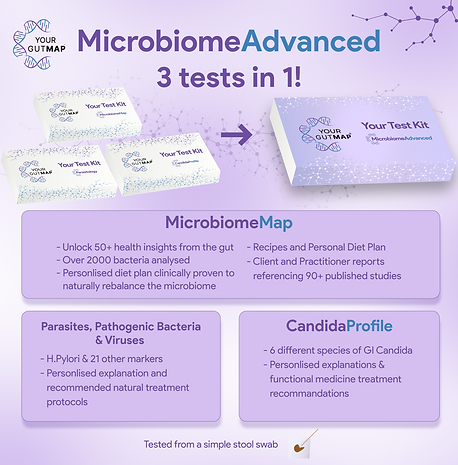
When traditional approaches fall short, microbiome testing offers a window into what's actually happening in your digestive system. Rather than treating all IBS the same way, it reveals your unique gut bacterial signature.

Testing shows exactly what's going on inside yor microbiome:
-
Which beneficial bacteria you're lacking (like Faecalibacterium, which reduces inflammation).
-
Which potentially troublesome bacteria are overgrown and cause IBS.
-
How your specific imbalance connects to your symptoms.
This approach doesn't just treat symptoms—it helps prevent future problems by addressing the underlying causes. You'll learn about lifestyle factors affecting your gut health and develop sustainable habits that keep things moving naturally.
Rather than depending on laxatives that your body can become dependent on, microbiome testing offers a path to restore your gut's natural rhythm through targeted nutrition, supplements, and lifestyle adjustments that make sense for your unique body.
This personalized insight transforms treatment from guesswork to precision. Instead of generic advice to "try cutting out dairy" or "eat more fiber," you'll learn:
-
Which specific foods feed your beneficial bacteria
-
Which foods might be triggering your symptoms
-
Which probiotics might help restore balance in your specific case
Some patients see remarkable improvements. For example, research shows that personalized microbiome-based dietary plans can improve symptoms in nearly 80% of patients within six weeks—far better than the one-size-fits-all approaches typically recommended.
Another recent research published in the American Journal of Gastroenterology and Gut Microbes Journal demonstrates that personalized dietary approaches based on Microbiome testing significantly outperform the standard low-FODMAP diet for managing Irritable Bowel Syndrome. The personalized approach not only proved less restrictive but delivered superior symptom relief, including a twofold reduction in pain and bloating severity. Patients following the personalized nutrition guide for six weeks experienced remarkable improvements: an 82% reduction in overall symptoms, fourfold decrease in IBS Severity Scale scores, and fivefold reduction in pain severity. Unlike the one-size-fits-all low-FODMAP diet, the personalized approach naturally balanced the gut microbiome, offering new hope for the estimated 20% of the population affected by IBS.
Beyond symptom relief, this approach helps prevent flare-ups by addressing underlying imbalances before they trigger a full episode. You might discover that your gut flora shifts before symptoms appear, giving you time to adjust your diet or supplements preventively.
Perhaps most importantly, microbiome testing shifts the focus from merely coping with IBS to actually addressing its root causes. By nurturing a healthier, more diverse gut ecosystem, you're not just treating symptoms—you're working toward lasting improvement in your digestive health and overall wellbeing.


Conventional treatment
There is no cure for syndrome in conventional medicine, only treatment of its symptoms.
Diarrhea is treated by prescribing drugs such as Loperamide (Imodium, Stop-it), constipation is treated with drugs such as Polyethylene glycol (Normalax, Peglax) while intestinal pain and spasms are treated with drugs such as Papaverine.
How Can Naturopathy Help?
My naturopathic approach for IBS focuses on balancing and strengthening the digestive system to reduce symptoms and improve overall digestive health.
Together, we identify dietary triggers and develop a balanced, personalised plan with all main food groups, soluble fibre, bioactive foods, essential vitamins, minerals, antioxidants, and fatty acids to promote healthy digestion, improve intestinal flora, and support regular bowel movements.
In our sessions, I guide you in adopting supportive eating habits—small, frequent meals, thorough chewing, and avoiding heavy or mixed meals that can strain digestion.
When food intolerance or sensitivity is suspected, we may use an elimination diet or the YourGutMap Food Sensitivity Test for precise results.
I often recommend the FODMAP diet, a low-carbohydrate plan that studies show can relieve IBS symptoms like bloating and abdominal pain by positively influencing gut flora.
Herbal treatments like peppermint oil are paired with stress-relieving practices tailored to your lifestyle for holistic symptom management.
Through regular consultations, I help you make adjustments, manage flares, and achieve sustainable digestive health, with a focus on long-term relief and enhanced well-being.
Everyone’s body and triggers are unique, which is why a personalised approach is essential to finding lasting relief and balance. If you have questions or would like to explore a tailored plan, please get in touch or book an introductory call to discuss how I can help.


Nutrition for IBS
The purpose of the nutritional treatment in treating irritable bowel syndrome is to balance and strengthen the digestive system and help improve the prevalence of the syndrome.
During the therapy sessions, I create a specific and balanced menu for the patient. A menu that contains all of the main food groups, dietary fiber (mainly soluble), bioactive foods, essential vitamins and minerals, antioxidants, and essential fatty acids, that will ease the digestive process, improve intestinal flora and contribute to a healthy and normal stool, reduce stomach pain and increase energy.
It is also important to keep in mind eating habits that include eating small meals at small intervals, prolonged chewing of the food, avoiding heavy meals, and separating between carbohydrates and proteins that facilitate digestion.
Many studies suggest a link between food intolerance and irritable bowel syndrome. Therefore, if there is a suspicion of food intolerance or hypersensitivity which may cause gastrointestinal irregularities, I usually recommend going on an elimination diet in order to identify the allergenic food.
Another amazing tool that I apply a lot when treating IBS, is FODMAP diet (low-carbohydrate diet). Some studies show that this diet can relieve irritable bowel symptoms such as bloating and abdominal pain. Such dietary intake has shown to produce changes in the composition of the bacteria in the intestinal flora, which may explain the positive effect of diet on my patients' irritable bowel syndrome.
FAQ
Have questions? We’ve gathered answers to some of the most common ones to help you on your wellness journey.

